Today we are launching our project toolkit – Bodies, Hearts, and Minds: Using the Past to Empower the Future. The toolkit uses historical sources to help young people think differently about their emotional and bodily wellbeing in the present, and their capacity to make change in the future.
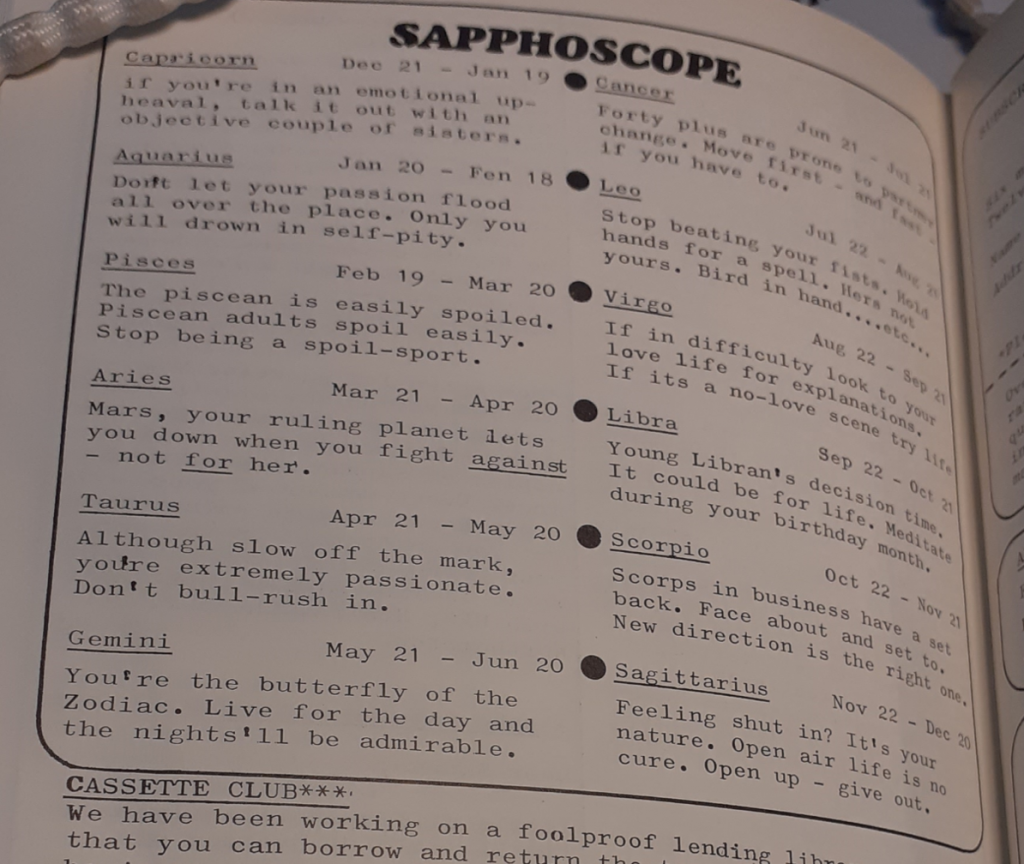
The toolkit is made up of activities that young people can carry out on their own or in groups. It is split into themes of ‘Generations’, ‘Growing Up’, ‘Body Image and Self-Expression’, and ‘Sex Education’. It includes a glossary of important terms, a list of resources to help young people start campaigning, and pointers to organisations that can provide support if they are experiencing problems.
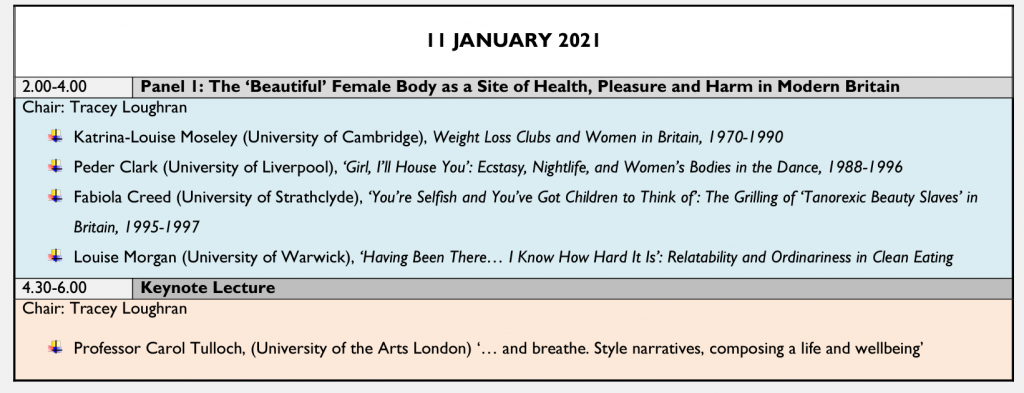
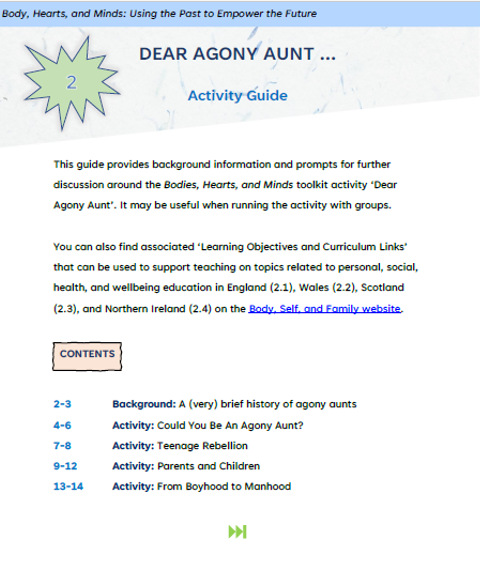
Accompanying the toolkit are resources for group leaders and teachers. Activity guides provide brief historical overviews, tips for running sessions, and ‘take home’ messages. These are complemented by sheets providing learning objectives and curriculum links for topics related to personal, social, and health education for England, Wales, Scotland, and Northern Ireland.
***
It has taken a long time, and help from lots of people, to create the toolkit. Back in 2017, when I was applying to the Wellcome Trust for funding for the Body, Self, and Family project, I didn’t know how to even start thinking about public engagement – What did I want to do? Who did I want to reach? What was I even capable of doing?
Talking to passionate, enthusiastic, and creative friends and colleagues about their work was inspirational (if also a little terrifying – these are seriously impressive people). Dave Wyatt’s CAER Heritage Project and SHARE with Schools, Dawn Mannay’s creative work with families and care-experienced young people, EJ Renolds’ AGENDA toolkit on positive relationships all showed what could be done at a grassroots level with enough determination.
Even after these conversations, I still had doubts. I wasn’t sure what I was capable of doing – I’d never really stepped outside my academic comfort zone before. I also wasn’t sure what I should work on. Dave, Dawn, and EJ all urged the importance of working on something that matters to you.

It took a while for the penny to drop. I eventually realised that I already spent a lot of time communicating about things I cared about enormously – in my undergraduate module on the history of gender, sexuality, and health in twentieth-century Britain. In this module, I tried to introduce students to topics that resonated with their present, and that helped them find different ways to negotiate a sometimes-hostile world. Why not try to reach younger people in similar ways?
***
This central aim never changed. But the sense of what the toolkit might achieve expanded a great deal over the next few years. Daisy Payling and Kate Mahoney, the postdoctoral researchers on the Body, Self, and Family project, brought their own considerable ideas, energies, and creativity. I often retreated to the background while they powered work on the toolkit. Its final form is a genuine act of co-creation.
It also bears the marks of all the people and organisations that worked with us. Daisy created and trialled activities at the University of Essex’s Digital Arts Festival, the Being Human Festival, the Annual LGBTQ+ History and Archives Conference, and the Royal College of Nursing Library and Archives/Surgery & Emotion Valentine’s Late. Kate went to Cardiff to run a focus group with the charity ACE (Action in Caerau and Ely). She spent multiple evenings driving around the furthest reaches of Essex to develop activities on period poverty and protest with Girl Guiding Groups, which she also ran with students at Colchester Academy. As we worked in these different contexts, we redrafted and refined the toolkit.
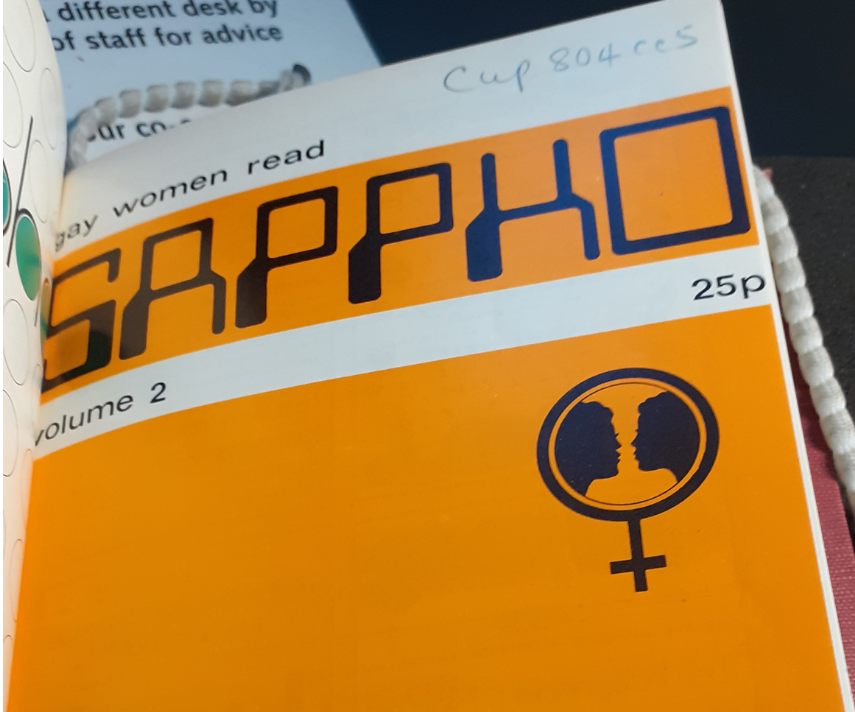
Our interactions with these different groups forced us to wrestle with difficult problems. We wanted the toolkit to show the reality of oppression in past and present societies. This is essential to validate struggles against racism, homophobia, and sexism. At the same time, we wanted to celebrate diverse voices and images – for young people to recognise themselves in the toolkit, and to understand their beauty and strength.
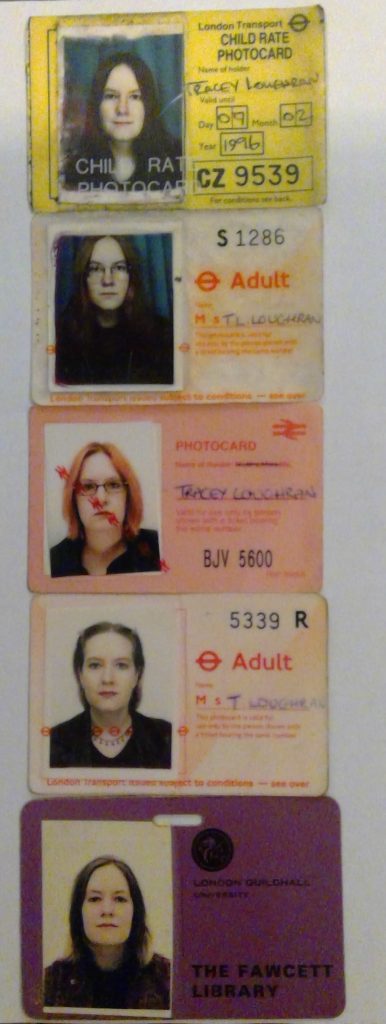
Working with historical sources made it especially difficult to balance these aims. One manifestation of power imbalances is the absence of representation in mass culture. How could this be shown in the toolkit? Simply finding exceptions to the rule of white heterosexual women and including them without comment presents a misleading picture – one that erases past racism and homophobia. But only discussing certain groups in terms of their oppression denies the joy in their identities and experiences.

We directly confronted these issues every time we encountered different audiences. As they asked us questions and shared their experiences, we renegotiated our own understandings of our responsibilities, and of the possibilities of the toolkit. In February 2020 we held a closed workshop to get further feedback on approaching these questions. Dawn Mannay, Priya Mistry, Khadija Osman, and Alison Twells provided invaluable guidance based on their own experiences of creative, artistic, and historical work with young people.
Our next step was to seek more formal feedback from our intended users of the toolkit – young people and group leaders, including teachers. The first lockdown in March 2020 made this more difficult than we had intended. Fortunately, Healthwatch Essex’s Young Mental Health Ambassadors were willing to trial our draft toolkit. Their feedback was hugely encouraging, but also made us confront some more difficult issues – not least that we needed more material aimed at all genders, not just girls.
Teachers also had insight that we lacked. Matthew Eggerton of Cardiff and Vale College, with extensive experience as a secondary school teacher, suggested that additional materials were needed to make it a truly useful resource. His guidance prompted us to produce activity guides, learning objectives, and curriculum links that help with lesson planning and delivery.
Now in the final stages of design, we commissioned activities that could plug the gaps in our own historical knowledge – mainly around young men’s experiences of health and wellbeing. Rich Hall contributed activities on generations in postwar Britain based on his research on fathers and sons; Mark Anderson put his scholarship on men’s hair to use in designing an activity on hair, schools, and stereotypes; and Katherine Jones supplied activities on masculinity and emotions, and sex education.
Around this time, we also read about Prim ‘N Poppin’. In this project, Julia Comita and Brenna Drury recreate vintage make-up advertisements to make them more inclusive. The resulting images tell us much about what – and who – is often missing in media depictions of beauty and fashion. The project responds to the dilemma about how to be inclusive while acknowledging social exclusion. We were thrilled when, with the permission of featured talent Cory and Kaguya, Julia and Brenna licensed us to use two Prim ‘N Poppin’ images.
There was still much work to do, but the toolkit now existed in a recognisable shape. Inspired by EJ Renolds’ AGENDA toolkit, we pulled together resources to help users find out about important issues, and work towards change. Natasha Richards pointed us towards organisations we had missed. Mindful of working with children who did not know what ‘menstruation’ meant, we also collaborated on a glossary. Finally, Kate produced a truly stunning design that perfectly represents the ethos of the toolkit – a DIY aesthetic that looks to the past but shapes it into something new; a powerful graphic that showcases the diversity and beauty of everyday lives.
***
It is strange to see the toolkit out in the world. It has been a background part of my working life for a long time. Writing about its creation reveals much about public engagement as a collaborative enterprise too. Daisy and Kate created the toolkit with my support, but so many other people have contributed along the way – in providing answers to our questions, but also in asking questions that we didn’t know needed answers; in inspiring us when we didn’t know where to start; and in encouraging us when we weren’t sure what to do next.
We believe the effort was worth it. It is important to know what happened in the past so that we can understand how we ended up where we are today. Knowing where we came from helps us to work out where we are going. Understanding how experiences of health and wellbeing were different in the past, especially what has changed and why, can help young people to think differently about the choices that are open to them.